Medical Management of Vascular Disease
![]()
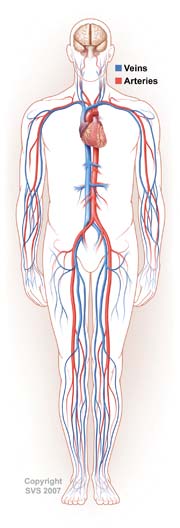 Atherosclerosis is a chronic, systemic disease which remains the leading cause of mortality and morbidity in the U.S. population. Patients with known peripheral vascular disease (PVD), including carotid artery, aortic, and lower extremity occlusive disease, are at elevated risk for cardiovascular death and disability.
Atherosclerosis is a chronic, systemic disease which remains the leading cause of mortality and morbidity in the U.S. population. Patients with known peripheral vascular disease (PVD), including carotid artery, aortic, and lower extremity occlusive disease, are at elevated risk for cardiovascular death and disability.
Cardiovascular Risk Reduction
Cardiovascular risk reduction is a primary component of treatment for all patients with PVD. This includes smoking cessation, weight reduction, diet, and lifestyle modifications. It also incorporates the use of athero-protective medications that are of proven benefit in vascular patients.
Treatment with a statin drug is indicated for all patients with PVD to achieve a target low density lipoprotein (LDL) level of <100 mg/dL. Level I evidence in support of this derives, most notably, from the Heart Protection Study, which demonstrated a 25 percent reduction in major cardiovascular events. In PVD patients considered to be at very high-risk, such as those with diabetes, metabolic syndrome, or multiple risk factors, a target LDL of 70 mg/dL is desirable.
In addition to reducing the long term risk of events, recent data suggests that statins may also be protective for vascular surgery patients in the perioperative period, though further evidence is needed. Pooled data from multiple large studies have established the excellent safety profile of these agents, though monitoring of liver function and clinical myopathy is appropriate.
Treatment of High Blood Pressure
Treatment of high blood pressure reduces the risk of major cardiovascular events. Antihypertensive medications should be used to achieve a blood pressure goal of less than 140/90 for nondiabetics and 130/80 for patients with diabetes or renal disease. Beta-blocker medications are effective for this purpose and are appropriate in the PVD population. ACE inhibitors are also effective antihypertensive agents whose cardioprotective effects may be independent of blood pressure lowering. Current guidelines suggest that ACE inhibitors are beneficial in all PVD patients including those without hypertension.
Antiplatelet Therapy
Lifelong antiplatelet therapy is also a cornerstone for all patients with established cardiovascular disease. Large meta-analyses have demonstrated a 20 to 25 percent reduction in major vascular events associated with antiplatelet use in PVD patients. Both aspirin and clopidogrel are protective. The CAPRIE study demonstrated an enhanced protective effect for clopidogrel over aspirin in PVD patients, however the cost-effectiveness of long-term clopidogrel is not established and it should primarily be considered as an aspirin alternative.
Diabetes and PVD
Diabetes is a potent risk factor for PVD and for increased cardiovascular risk. Aggressive treatment of diabetes reduces the risk of microvascular complications such as retinopathy and nephropathy. Monitoring of glycemic control to achieve Hgb A1C levels less than 7 percent is currently recommended. All vascular specialists need to be familiar with guidelines for risk factor modification and medical management to reduce the long term sequelae of atherosclerosis in our patients. Ongoing and future studies will continue to define the optimal dosing, treatment targets, and potential role of combination drug therapies in the PVD population.
